From birth some individuals are born with structural heart abnormalities, known as congenital heart defects (CHDs). While many with CHDs can enjoy active lives, the risk of complications, such as sudden cardiac arrest (SCA), can be elevated by certain defects. Early detection, management, and preventative measures are critical; hence, understanding this connection is essential. This article explores the relationship between CHDs and SCA, looking at defect types, risk factors, prevalence, and ways to prevent SCA.
What Defines a Congenital Heart Defect?
A wide array of structural heart issues fall under the umbrella of congenital heart defects. These abnormalities happen during fetal development, potentially affecting the heart’s chambers, valves, or major blood vessels. CHDs are, in fact, the most common type of congenital disability, affecting about 1% of live births.
Various Congenital Heart Defect Types
Classifying CHDs is possible; each category presents its unique characteristics and potential complications.
Septa/Atrial Septal Defects Explained
Septal defects involve holes in the walls (septa) separating the heart’s chambers. Common examples include:
Atrial Septal Defect (ASD): A hole between the heart’s two upper chambers (atria).
Ventricular Septal Defect (VSD) is a hole between the heart’s two lower chambers (ventricles).
Understanding Obstruction Defects
Obstruction defects relate to narrowed heart valves or vessels restricting blood flow. For instance:
- Pulmonary Stenosis is the narrowing of the pulmonary valve, which regulates blood flow from the heart to the lungs.
- Aortic Stenosis: Narrowing occurs in the aortic valve, which controls blood flow from the heart to the body.
- Coarctation of the Aorta: The aorta narrows; this main artery carries blood from the heart.
Cyanotic Defects: Key Details
Blood oxygen levels drop because of cyanotic defects, resulting in cyanosis (a bluish tint). Examples are:
- Tetralogy of Fallot: A combination of VSD, pulmonary stenosis, an overriding aorta, and right ventricular hypertrophy.
- Transposition of the Great Arteries (TGA): The aorta and pulmonary artery are switched, creating separate circulations of oxygen-poor and rich blood.
What Causes Congenital Heart Defects?
Many CHD causes remain unknown. However, factors like these appear to increase the risk:
- Genetic Factors: CHDs sometimes link to genetic syndromes like Down syndrome or Turner syndrome.
- Environmental Factors: Exposure to certain medications, infections (such as rubella), or substances (like alcohol or drugs) during pregnancy.
- Maternal Health Conditions: Diabetes or lupus in the mother could increase CHD risk in the baby.
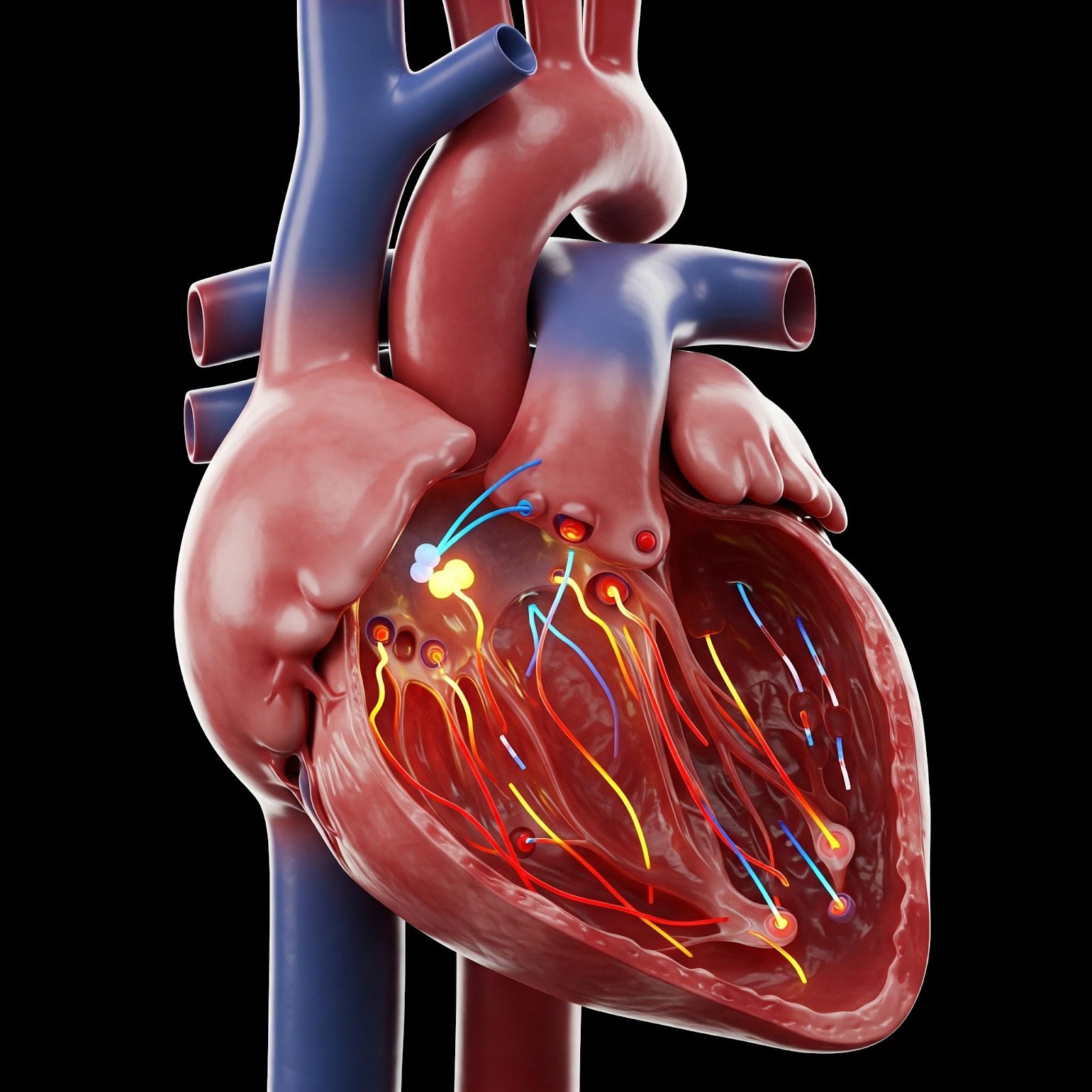
Sudden Cardiac Arrest: A Definition
Sudden cardiac arrest (SCA) is a sudden and unexpected loss of heart function, breathing, and consciousness. Usually, it’s an electrical disturbance disrupting the heart’s pumping, stopping blood flow to vital organs. Immediate treatment is required, including CPR and defibrillation, because SCA is a medical emergency.
Sudden Cardiac Arrest: Common Causes
SCA can result from several factors, including:
- Coronary Artery Disease: Arteries that supply blood to the heart are blocked.
- Cardiomyopathy: Diseases affecting the heart muscle itself.
- Heart Valve Problems: Problems are present with the heart valves regulating blood flow.
- Electrical System Abnormalities: Issues with the heart’s electrical system, like long QT syndrome.
Symptoms Indicating Sudden Cardiac Arrest
Often, SCA occurs without warning. However, some might have symptoms beforehand, like:
- Chest Pain: Discomfort or pressure felt in the chest.
- Shortness of Breath: Difficulty or feeling unable to get enough air.
- Dizziness or Lightheadedness: A feeling of faintness or unsteadiness.
- Palpitations: Sensations of rapid, fluttering, or pounding heartbeats.
Connecting Congenital Heart Defects to SCA.
Certain congenital heart defects (CHDs) can elevate the likelihood of sudden cardiac arrest (SCA), generally speaking, due to the structural or electrical irregularities they present. These irregularities may disrupt the heart’s rhythm or compromise its ability to pump blood effectively, which can lead to SCA.
How, then, do CHDs, specifically, increase the risk of SCA? There are, in most cases, several ways:
- Abnormal Heart Rhythms (Arrhythmias): As mentioned, structural defects can disturb the heart’s complex electrical system, precipitating arrhythmias. Arrhythmias are known to sometimes trigger SCA.
- Reduced Blood Flow: Obstruction-type defects, or indeed those that cause the undesirable mixing of oxygen-poor with oxygen-rich blood, may diminish the heart’s pumping efficacy, thus elevating SCA risk.
- Increased Pressure on the Heart: Defects leading to augmented pressure within the heart’s chambers can potentially induce heart failure, a known risk factor when considering SCA.
Figuring out the precise prevalence of SCA among those with CHDs is, however, challenging. This is partly because of variations in defect type and severity, alongside differences in reporting methods. Yet multiple studies do indicate that individuals with particular CHDs face a substantially increased SCA risk compared to the population at large.
Specific CHDs and SCA Risk
Some specific CHDs are associated with a higher SCA risk.
| CHD Type | Description | Increased SCA Risk |
|---|---|---|
| Tetralogy of Fallot | A combination of four heart defects | Moderate to High |
| Transposition of the Great Arteries | Switched positions of the aorta and pulmonary artery | Moderate to High |
| Anomalous Coronary Arteries | Coronary arteries originate from the wrong place | High |
| Long QT Syndrome | Electrical abnormality causing prolonged QT interval | High |
| Hypertrophic Cardiomyopathy | Thickening of the heart muscle | High |
Influencing Factors for SCA Risk
Several factors influence SCA risk in individuals already diagnosed with CHD. These might include:
- Type and Severity of CHD: The specific nature and severity of the heart defect are important in evaluating overall risk.
- Age at Diagnosis and Treatment: If diagnosis and subsequent treatment occur early, that can significantly lower the incidence of complications (SCA being one).
- Presence of Other Medical Conditions: Other pre-existing medical issues (diabetes, kidney disease, etc.) may increase the risk.
- Lifestyle Factors: Consider smoking, obesity, and even a lack of exercise; these are risk factors to consider.
So, how can one approach prevention and overall management of SCA in CHD patients?
Early Diagnosis and Treatment:
CHD early diagnosis, facilitated through prenatal screening or newborn examinations, is essential. Post-diagnosis, appropriate treatment (surgery, medication, or other interventions) can then manage the defect itself and, in turn, lower complication risks.
Ongoing Monitoring and Management
Ongoing monitoring is needed, overseen by a cardiologist. Expect regular check-ups, echocardiograms, electrocardiograms (ECGs), and other relevant tests. The goals are to assess heart function and watch for possible issues.
Lifestyle Modifications
Lifestyle adjustments may also reduce the risk. For example:
Regular Exercise: If it is under guidance from a cardiologist, of course.
Healthy Diet: A balanced diet low in saturated fats and sodium.
Avoiding Smoking and Excessive Alcohol Consumption: Steer clear of any habits that might negatively affect your heart.
Stress Management: Consider meditation, yoga, and other stress-reducing techniques.
Implantable Cardioverter Defibrillators (ICDs)
Sometimes, ICDs become relevant for high-risk individuals. These are small devices implanted under the skin that monitor the heart’s rhythm. If an arrhythmia is detected, an electric shock is delivered.
Emergency Preparedness
Having an emergency plan is essential.
CPR Training: Learn CPR to save lives.
Having Access to an AED: Make sure automated external defibrillators (AEDs) are portable and readily available.
Defibrillators, which are devices used to restore a normal heart rhythm by delivering an electric shock, play a crucial role.
Knowing when to call emergency services—it’s absolutely vital to call immediately at the first indication of SCA.
Living with a Congenital Heart Defect
Living with a CHD can present challenges. However, with appropriate care and support, people can lead fulfilling lives.
Support Groups and Resources
Support groups and resources can provide emotional and practical assistance to individuals with CHD and their families. These resources offer information, connect individuals facing similar challenges, and guide condition management.
Psychological Support
Dealing with a chronic ailment can cause emotional distress. Psychological support is crucial for individuals with CHD. Therapy or counseling helps people manage stress and anxiety.
Transitioning to Adult Care
Adolescents with CHD will have to transition from pediatric to adult care. Locating an adult cardiologist who is experienced is vital.
Author: Donna Ryan lives and works in Tucson, AZ.